Resistance to antibiotics was on Wednesday declared a “major global threat” to public health by the World Health Organization in a first-ever global surveillance report that collated data from 114 countries.
It said some superbugs have evolved so much that up to 50% of the affected patients don’t get cured by drugs commonly used against them. Common microbes such as E coli, for instance, are posing a major emergency in intensive care units across the world.
“Without urgent, coordinated action by many stakeholders, the world is headed for a post-antibiotic era in which common infections and minor injuries which have been treatable for decades can once again kill,” said WHO’s Dr Keiji Fukuda while releasing the report.
The report had a special warning for India. “The infectious disease burden in India is among the highest in the world and the inappropriate, irrational use of antimicrobial agents against these diseases has led to an increasing trend in development of antimicrobial resistance,” it said. The report — Antimicrobial Resistance: Global Report on Surveillance — studied antibiotic resistance in nine different bacteria responsible for common diseases such as sepsis, diarrhoea, pneumonia, urinary tract infections and gonorrhoea.
Failure of the last resort of treatment for gonorrhoea — third generation cephalosporins — has been confirmed in Austria, Australia, Canada, France, Japan, Norway, Slovenia, South Africa, Sweden and the UK. Over 1 million people are infected with gonorrhoea around the world every day.
Said an intensivist in a south Mumbai hospital, “An increasing number of patients who reach the ICU with urinary tract infection are resistant to normally prescribed medicines.” The doctor said the medical fraternity couldn’t depend on one antibiotic alone. “We are using drugs in combinations most of the time.”
The WHO report found half the patients treated for sepsis caused by K pneumoniae don’t respond to carbapenem antibiotics. It also noted that fluoroquinolones used for urinary tract infections caused by E coli, don’t work in 50% cases. “In the 1980s, when fluoroquinolones were introduced, resistance was virtually zero. Today, there are countries where this treatment is ineffective in more than half of patients,’’ the report noted.
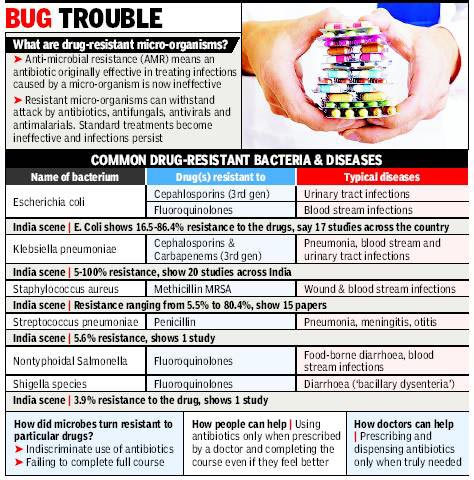
It stressed that antibiotic resistance was causing people to be sicker for a longer time and increasing the risk of death. “People with MRSA (methicillin-resistant Staphylococcus aureus) are 64% more likely to die than people with a non-resistant form of the infection,’’ it said.
In India, the emergence of extremely drug resistant TB drove home the extent of antibiotic resistance. Mumbai’s doctors had in 2011-2012 highlighted TB cases that were resistant to all the known antibiotics usually used to treat it. WHO, in 2011, estimated that there are 6.3 lakh cases of multi-drug resistant tuberculosis (MDRTB) among the world’s 12 million cases of TB.
The WHO report blamed poor regulation in the medical sector, with respect to prescription, in India.
Source
Times Of India
01 May 2014
Pune, India
TIMES NEWS NETWORK






